Borderline Personality Disorder
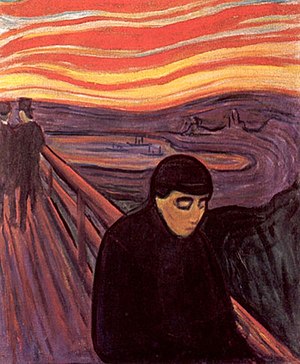
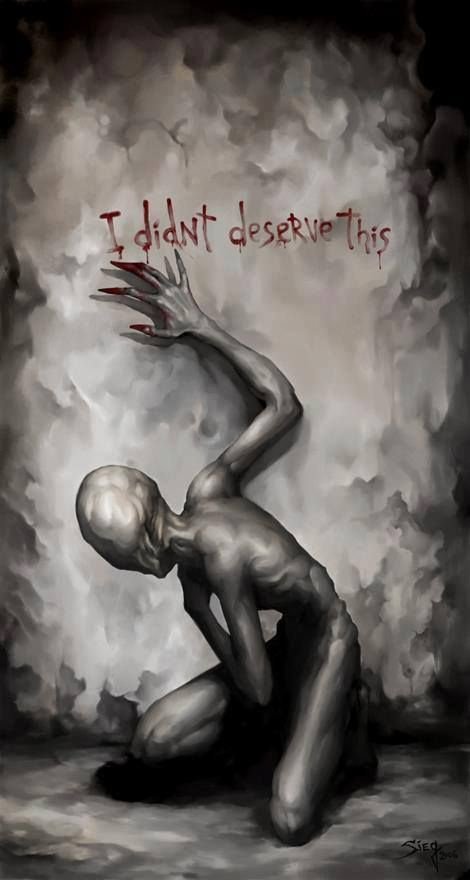
Borderline personality disorder (BPD), also known as emotionally unstable personality disorder (EUPD),[11] is a personality disorder characterized by a long-term pattern of unstable interpersonal relationships, distorted sense of self, and strong emotional reactions.[12][7][13] Those affected often engage in self-harm and other dangerous behaviors, often due to their difficulty with returning their emotional level to a healthy or normal baseline.[14][15][16] They may also struggle with a feeling of emptiness, fear of abandonment, and detachment from reality.[12] Symptoms of BPD may be triggered by events considered normal to others.[12] BPD typically begins by early adulthood and occurs across a variety of situations.[7] Substance use disorders, depression, and eating disorders are commonly associated with BPD.[12] Some 8 to 10% of people affected by the disorder may die by suicide.[12][7] The disorder is often stigmatized in both the media and the psychiatric field and as a result is often underdiagnosed.[17]
The causes of BPD are unclear but seem to involve genetic, neurological, environmental, and social factors.[6][8] It occurs about five times more often in a person who has an affected close relative.[6] Adverse life events appear to also play a role.[9] The underlying mechanism appears to involve the frontolimbic network of neurons.[9] BPD is recognized by the American Diagnostic and Statistical Manual of Mental Disorders (DSM) as a personality disorder, along with nine other such disorders.[7] The condition must be differentiated from an identity problem or substance use disorders, among other possibilities.[7]
BPD is typically treated with psychotherapy, such as cognitive behavioral therapy (CBT) or dialectical behavior therapy (DBT).[6] DBT may reduce the risk of suicide in the disorder.[6] Therapy for BPD can occur one-on-one or in a group.[6] While medications cannot cure BPD, they may be used to help with the associated symptoms.[6] Quetiapine and SSRI antidepressants remain widely prescribed for the condition, though there is no evidence regarding the efficacy of the latter class of drugs.[18] Severe cases of the disorder may require hospital care.[6]
About 1.6% of people have BPD in a given year, with some estimates as high as 6%.[6][7][19] Women are diagnosed about three times as often as men.[7] The disorder appears to become less common among older people.[7] Up to half of those with BPD improve over a ten-year period.[7] Those affected typically use a high amount of healthcare resources.[7] There is an ongoing debate about the naming of the disorder, especially the suitability of the word borderline.[6]
BPD is characterized by nine signs and symptoms. To be diagnosed, a person must meet at least five of the following:[20]
- Frantic efforts to avoid real or imagined abandonment
- Unstable and chaotic interpersonal relationships, often characterized by alternating between extremes of idealization and devaluation, also known as “splitting“
- Markedly disturbed sense of identity and distorted self-image[6]
- Impulsive or reckless behaviors (e.g., impulsive or uncontrollable spending, unsafe sex, substance use disorders, reckless driving, binge eating)[21]
- Recurrent suicidal ideation or self harm
- Rapidly shifting intense emotional dysregulation
- Chronic feelings of emptiness
- Inappropriate, intense anger that can be difficult to control
- Transient, stress-related paranoid or severe dissociative symptoms
Overall, the most distinguishing symptoms of BPD are pervasive patterns of instability in interpersonal relationships and self-image, alternating between extremes of idealization and devaluation of others, along with varying moods and difficulty regulating strong emotional reactions. Dangerous or impulsive behavior is also correlated with the disorder.
Other symptoms may include feeling unsure of one’s identity, morals, and values; having paranoid thoughts when feeling stressed; depersonalization; and, in moderate to severe cases, stress-induced breaks with reality or psychotic episodes. Individuals with BPD often have comorbid conditions, such as depressive and bipolar disorders, substance use disorders, eating disorders, post-traumatic stress disorder, and attention-deficit/hyperactivity disorder.[20]